Hi friends! Let’s talk about a scary gap that’s opening up in healthcare. Imagine you have what you think is incredible insurance—maybe even a policy with a $5 million lifetime limit. Now imagine you get a cancer diagnosis, and your doctor says the most promising treatment is a new, smart drug designed by artificial intelligence. You’d assume you’re covered, right? Well, a growing number of patients are getting a devastating surprise: a denial letter citing an “experimental treatment exclusion.” This isn’t a distant future problem; it’s a 2026 reality that’s catching even the well-insured off guard. Today, we’re going to pull back the curtain on this insurance trap, explain why it’s happening now, and most importantly, give you a clear action plan to protect yourself and your family.
The core of the problem is a specific clause buried in your policy’s fine print. This article will uncover how insurers are using this old rule in a new way to deny coverage for next-generation AI cancer drugs, creating a perfect storm of medical hope and financial despair.
Deconstructing the Experimental Treatment Exclusion: The Fine Print That Never Went Away
First, let’s understand the weapon in question. The “Experimental or Investigational Treatment” exclusion is a standard feature in most health insurance policies. It’s not new. For decades, its purpose was straightforward: to prevent insurers from paying for treatments that are not widely accepted by the medical community, lack sufficient peer-reviewed evidence, or are essentially untested. It was a cost and risk management tool designed, in principle, to steer patients toward proven care.
Insurers typically judge a treatment against criteria like its FDA approval status, the strength of evidence in major medical journals, its inclusion in recognized treatment guidelines (like those from the National Comprehensive Cancer Network), and whether it’s considered the “standard of care” for a condition. Historically, this created a clear line: FDA-approved drug? Usually covered. Not FDA-approved? Usually not. Medical insurance exclusions like this have long been a feature of the landscape, covering everything from cosmetic surgery to injuries from hazardous activities, as noted in general overviews of policy limitations.
For a long time, this system worked predictably. But the revolutionary pace of AI in medicine is blurring those once-clear lines into a confusing gray area. The single most important shift is that insurers are now applying this old exclusion to brand-new categories of FDA-approved treatments, fundamentally changing the risk for patients.
This strategic narrowing of coverage isn’t limited to cancer drugs. A similar battle is unfolding over access to another breakthrough—and costly—class of medications.
Why AI Drugs Are the Perfect Target for This Exclusion
Artificial intelligence is revolutionizing drug discovery. It can sift through billions of data points to identify novel drug candidates, predict their efficacy, and even repurpose existing drugs for new cancer treatments in a fraction of the traditional time. But this speed creates a critical vulnerability when it collides with insurance policy language.
The core issue lies in the regulatory pathway. To get life-saving drugs to patients faster, the FDA often grants “Accelerated Approval” based on promising early data (like tumor shrinkage). However, the drug company must still run confirmatory trials to prove it actually extends or improves life—this leads to “Traditional Approval.” For AI-accelerated drugs, this creates a dangerous limbo: they are FDA-approved, but not *fully* approved in the eyes of an insurer looking for long-term survival data. Insurers are actively exploiting this gap, arguing the drugs lack “sufficient evidence” of clinical benefit, which is the exact language of the experimental treatment exclusion. This isn’t theoretical; it’s already happening, as seen in cases where an insurer denies access to drugs granted accelerated approval by the FDA.
| Phase | Traditional Drug (10+ years) | AI-Accelerated Drug (5-7 years) | Insurer’s Perspective in 2026 |
|---|---|---|---|
| Pre-Clinical | Years of lab research | AI simulation & modeling in months | ‘Highly Investigational’ |
| Clinical Trials (Phases I-III) | Sequential, large-scale trials | Smaller, adaptive trials using predictive biomarkers | ‘Limited patient population data’ |
| FDA Approval | Full Approval based on overall survival data | Often Accelerated Approval based on surrogate endpoints (e.g., tumor response) | ‘Lacks conclusive survival benefit evidence’ |
| Post-Market | Long-term safety monitoring | Confirmatory trial ongoing for Full Approval | ‘Still considered investigational until trial completes’ |
This table shows the mismatch. The evidence timeline for breakthrough AI cancer drugs simply doesn’t align with the slow, traditional yardstick many insurers are using to define “investigational.”
The 2026 Payer Playbook: How Insurers Are Justifying Denials
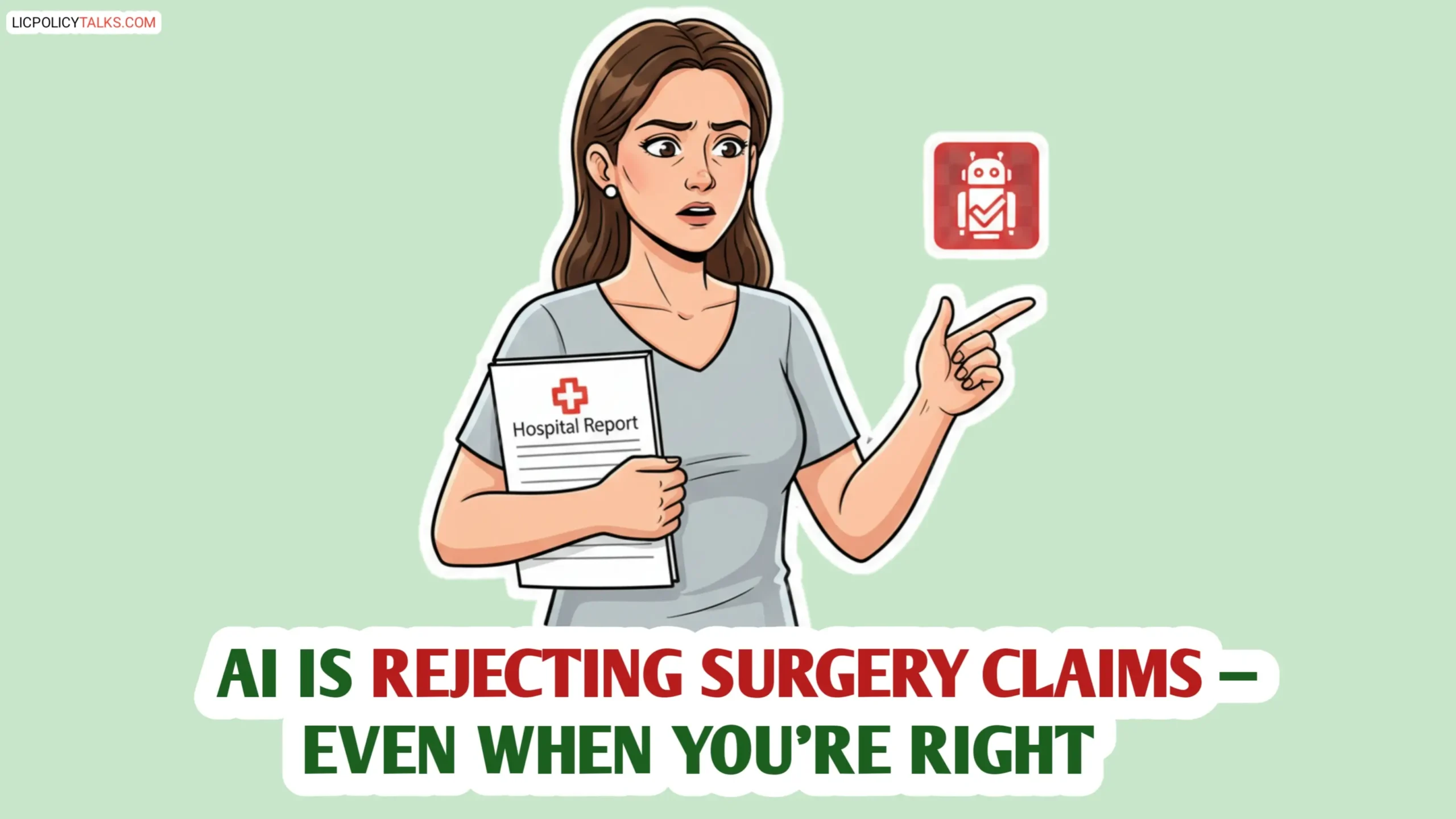
Looking ahead to health insurance 2026, this isn’t about random denials; it’s a strategic shift. Insurers are updating their internal clinical policies to specifically tighten evidence requirements for high-cost oncology drugs, especially those on accelerated pathways or with novel, AI-derived mechanisms. Internal “Formulary Committees” are increasingly empowered to label a drug as “investigational” even after it receives an FDA nod, essentially second-guessing the regulator.
The result is a sharp increase in claim rejections for the most advanced therapies. While traditional treatments see low denial rates, the newest weapons in the fight against cancer are being systematically flagged. The following projection, based on analysis of industry trends and reports like the one from Forbes on accelerated approval denials, illustrates the looming disparity in insurance coverage.
Projected Claim Denial Rates for Novel Oncology Drugs (2024-2026)
Based on industry analysis of payer policy trends. Denial rate for AI drugs reflects the high risk of the “experimental” designation.
Fighting Back: A Patient’s Step-by-Step Guide for 2026 and Beyond
Knowledge is your first line of defense. You don’t have to be a passive victim of this insurance denial trend. Here is a proactive, step-by-step guide to secure treatment access.
Step 1: Audit Your Policy *Now*. Don’t wait for a crisis. Dig out your full policy document (the Summary Plan Description or SPD). Use the “Find” function to search for keywords: “experimental,” “investigational,” “unproven,” and “medical necessity.” Understand the exact language that could be used against you.
Step 2: Master the Appeal. If you get a denial, appeal immediately. Build a powerful “medical necessity” case with your doctor. Gather letters of support, relevant clinical trial data, and citations from major cancer treatment guidelines (like NCCN) that endorse or mention the drug. Be prepared for multiple appeal levels, both internal and external.
Step 3: Explore Financial Safeguards. Investigate supplemental plans like Hospital Indemnity or Critical Illness policies, which pay lump sums upon diagnosis. CAUTION: These often have their own exclusions, so read their fine print just as carefully. Understanding policy details is crucial, whether for people or pets—it’s why knowing how pet insurance works is a useful analogy for grasping reimbursement models and loopholes.
Step 4: Leverage Advocacy. You are not alone. Connect with patient advocacy groups specific to your cancer type. They often have resources, template appeal letters, and knowledge of which insurers are more resistant. Legal aid organizations specializing in healthcare can also provide guidance.
The single most important action you can take is to have the “what if” conversation with your oncologist before starting a novel therapy. Ask them, “Based on your experience, is this drug likely to trigger an experimental treatment exclusion with my insurer, and how can we preemptively build our case?”
Fighting coverage denials is one front in this war. Patients also need to guard against another modern threat: surprise billing for the AI-assisted procedures themselves.
The Policy Battlefield: What’s Being Done (And Not Done)
This fight is also happening at the legislative level. Some states and federal lawmakers have proposed bills to mandate insurance coverage for drugs with FDA Accelerated Approval, trying to close the loophole. However, these efforts face fierce resistance from insurance lobbies, who argue about unsustainable costs and the principles of “evidence-based medicine.”
Another key player is your employer. Companies that choose group health plans for their employees have immense power to demand policies with broader, more forward-thinking coverage for novel therapies. As an employee or a benefits manager, this is a critical conversation to start.
It’s worth noting that targeted policy exclusions are not a new tactic in healthcare policy. Similar battles have been fought over coverage for specific groups, where access to care is blocked by precise wording, much like how the experimental label is being used now. Systemic change is slow. While the policy wheels turn, your immediate and most powerful recourse is the personal vigilance outlined in the steps above.
FAQs: ‘insurance denial’
Q: If an AI-developed cancer drug has FDA Accelerated Approval, isn’t it illegal for my insurer to deny it?
Q: I have a ‘Cadillac’ health plan through my employer. Am I still at risk for these denials?
Q: What’s the single most important question I should ask my insurance provider today?
Q: Are there any insurance companies known for having more favorable coverage policies?
Q: If my appeal is denied, what are my last-resort options for accessing these treatments?
Beyond the Fine Print: Redefining Preparedness in the Age of AI Medicine
The stark reality is that a $5 million insurance policy is no longer a guaranteed ticket to the best available care. The financial risk has subtly shifted from the total cost of care to the scope of what’s covered. The old rules of thumb no longer apply in the era of AI-driven medicine.
The solution is a three-part shield: personal policy literacy, proactive financial planning, and collective advocacy. Understanding the experimental treatment exclusion is no longer about deciphering obscure legalese for the curious—it’s a critical component of managing your health and financial survival. As AI cancer drugs become more common, your awareness and preparedness will determine your access to them. Don’t let the fine print define your future.